This research explores the application of 3D printing and scanning technologies in the development of customised ventilation face masks for very young infants and children.
Funders: National Institute for Health Research (NIHR)
Partners: Sheffield Teaching Hospitals, Sheffield Children’s Hospital, Devices4Dignity, Medipex, Materialise NV/UK
Project team: Heath Reed, Matt Willox, Naomi Raszyk, Joe Langley, Julie Roe

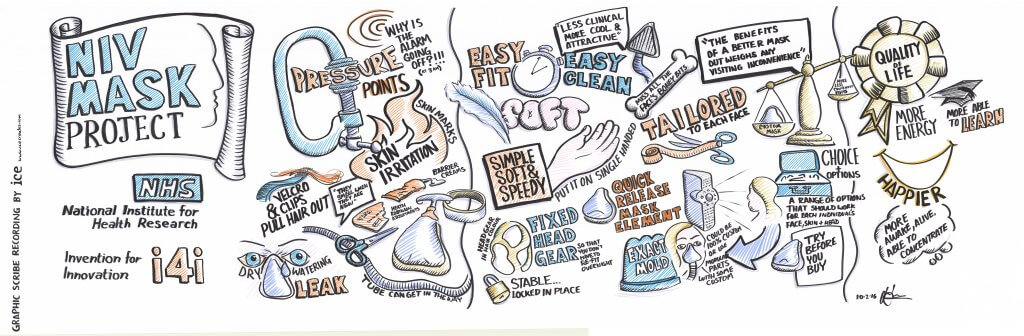
Non-invasive ventilation (NIV) is the delivery of breathing support via a face-mask. It is used to treat individuals whose breathing is compromised. Evidence shows that when used long term it improves quality of life and life expectancy. Mass produced masks are available for adults but in children it is often difficult to find a mask that provides an adequate seal. Current options for children are to ventilate invasively via a breathing tube, to persevere with NIV through an inadequate mask or to abandon ventilation.

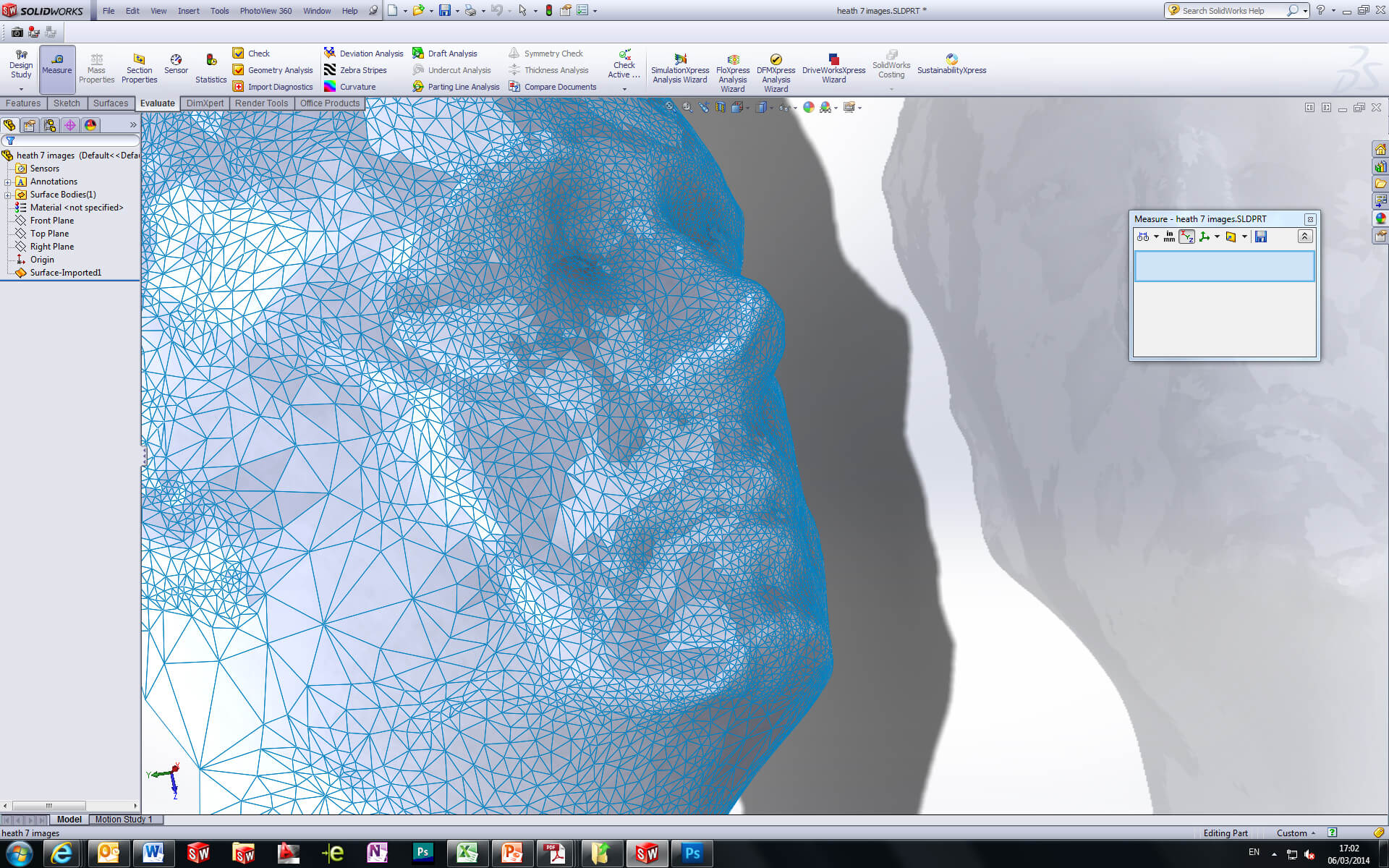
This research explores the application of 3D printing and scanning technologies within the NHS to enable the delivery of customised face mask for infants and children. Participatory research methods involving children and parents have helped specify techniques and processes that could be used to deliver novel mask-face interfaces in a way that suits the needs of individual patients.
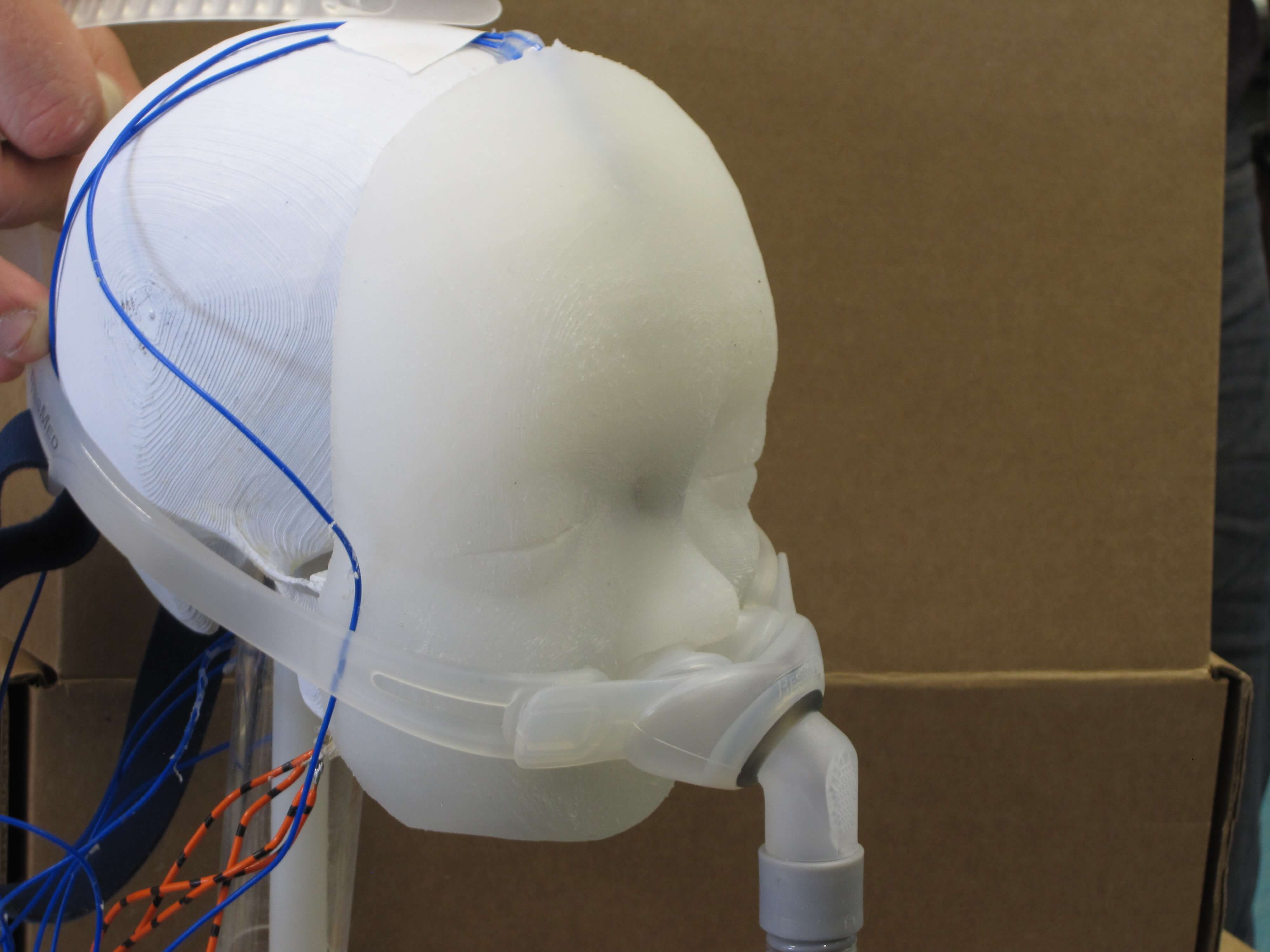

To date, lab testing has demonstrated that the methodology and pre-production prototypes are more effective than standard mass produce masks that are currently available.
A critical part of the initial development and proposals was the active involvement of patients, their close families, and wider affected communities and organizations through specific focus group interactions. This includes, for example a parent who is now a member of the research programme team.
To further support the speed of future implementation and good concurrent practice, effective links with industries have been made. We have engaged with both a large global (Phillips Respironics) and a UK based manufacturer of NIV devices (B&D Electromedical), both of whom are enthusiastic in their support for the project. Materialise, who make 3D scanning systems and 3D printing technology, have joined the project team. Together these businesses can provide the relevant understanding of the practicalities of the ventilation business and of the materials, manufacturing and regulatory challenges involved in the project. As part of this concurrent phase of the research and development R&D we are also investigating potential business models appropriate for a national and international market.
The results should also be transferable to adult medicine, whereby the potential commercial impact and savings to the NHS could be substantial.
Heath Reed
In tests, 73% patients reported comfort and fit that was as good or better than their usual mask.
Health economics have demonstrated that a custom-made mask would be cost effective at a price below £500.
 to top
to top
