Patient experience is a highly contested concept. However there is emerging evidence and near universal agreement that Patient Experience (PE) feedback is necessary in order to deliver high quality care. In the UK, there is a mandatory requirement to capture patient experience data. This project aimed to explore staff attitudes towards and understanding of patient experience data, and what (if anything) they did with it.
Funded by NIHR HS&DR
Partners:
Bradford Institute of Health Research
NIHR CLAHRC YH
Project Team:
Design Lead – Joe Langley
Rebecca Partridge, Ian Gwilt, Rebecca Lawton, Laura Sheard, Claire Marsh

An initial scoping review was conducted in stage 1 to understand what Patient Experience (PE) measures are currently collected, collated, and used to inform service improvement and care delivery.
Stage 2 was a phase of action research and co-design iteratively combined. This was followed by an evaluation and a refinement of the intervention developed in stage 2 for scale up to the wider NHS context.

Our specific contribution focused on the co-design in stage 2.
A patient experience improvement toolkit was developed through three workshops using participative co-design methods. Representatives from six wards from three NHS Trusts and a group of six patient/public representatives volunteered to take part in the three workshops. Members of the research team (who did the initial scoping research) also participated in the co-design.
The initial prototype was piloted for a 12 month period through an embedded action researcher process. The action researchers then engaged in a subsequent design consultancy process to refine and modify the toolkit.
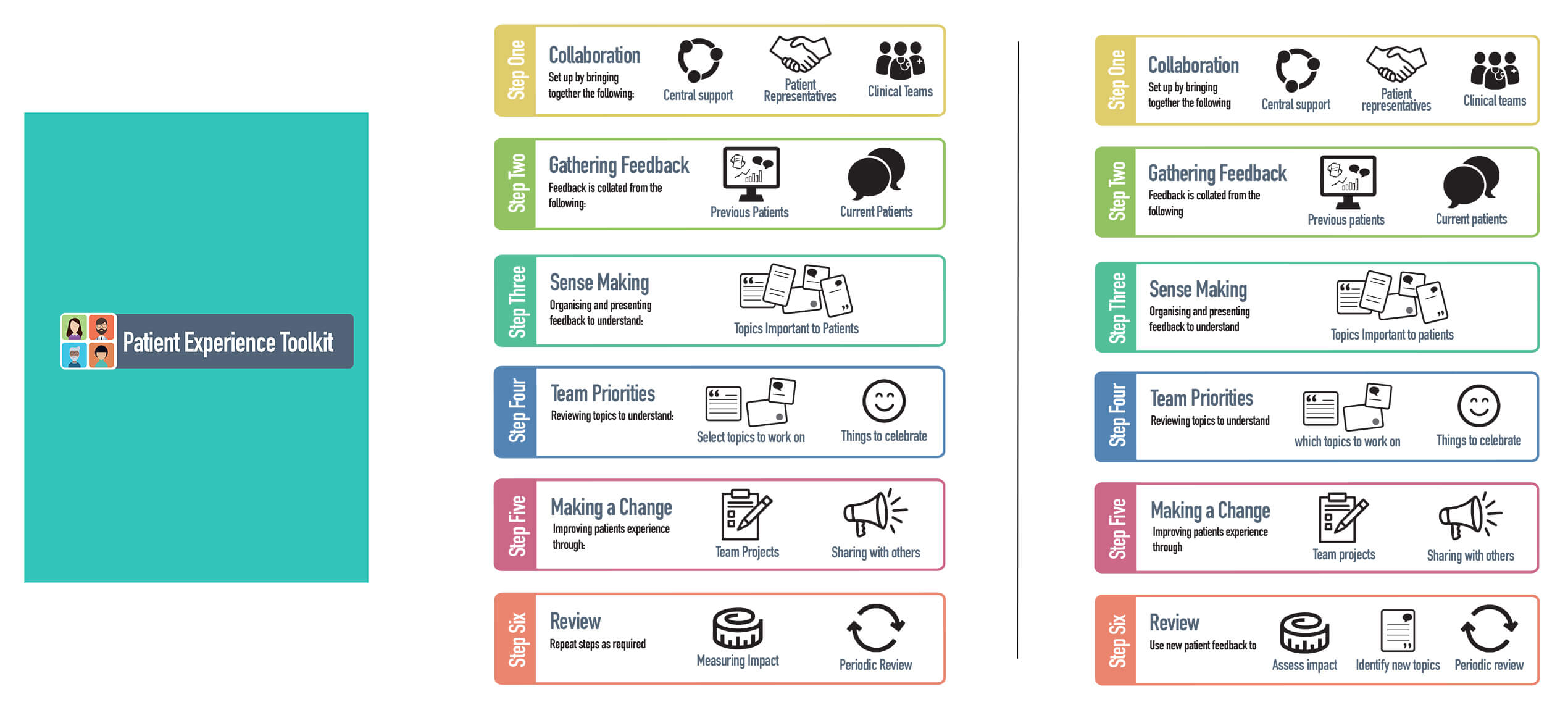
A toolkit was developed to support frontline staff to access, collect, analyse, interpret and use patient experience data to identify ward level changes prototypes and sustain them.
It was identified that the data interpretation skills did not typically exist in the ward and so the toolkit was modified to accommodate a data skilled person as a toolkit facilitator. This individual took on many of the characteristics of the action researchers – primarily because the action researchers took up this role in order to keep the project moving forwards.
What was interesting from a co-design and design research perspective was the presence of the action researchers in the extended prototype testing phase and the mediating role that the action researchers took on after this, acting as an intermediary and gatekeeper between the design team and the frontline staff who had tested the toolkit.
This raised interesting questions for us about how to access the right knowledge (from the frontline staff) ‘remotely’ and how to design ‘around’ the action researchers – in our minds was a constant query about the influence the action researchers played in the process and became part of the intervention itself.
Higher order reflections about design researchers working with health sciences researchers and the integration of methods from design research and health sciences were also raised.
The toolkit has since been further refined into the Yorkshire Patient Experience Toolkit (YPET). A coaches network has been established to support ward staff to use the toolkit, and is available as a free resource.
 to top
to top
