Parkinson’s Disease (PD) is a highly complex progressive neurodegenerative disease. Individuals experience PD in a wide variety of ways, leading to difficulty in diagnosis, acceptance and on-going management. Service provision is complex and varied depending on provider. This project utilised a participatory design methodology to identify patient and provider needs for PD services in the South West Peninsula. Then used co-design to develop tools, resources and service structures to meet these.
Funded by :
Bial Pharmaceuticals
University Hospitals Plymouth NHS Foundation Trust
Sheffield Hallam University
Partners:
University Hospitals Plymouth NHS Foundation Trust
Sheffield Hallam University
Livewell Southwest
People living with Parkinson’s Disease and their family’s/carers
Parkinson’s UK
Project team:
Joe Langley
Rebecca Partridge
Parkinson’s occurs when a small group of nerve cells in the brain no longer produce enough dopamine. This is a chemical that transmits messages from the brain to other parts of the body, enabling people to perform smooth, coordinated movements. Insufficient dopamine messes up these transmissions. Although typically associated with tremors, muscle stiffness and slower movements, it is also associated with a wide range of other symptoms including nightmares and night sweats, hallucinations, reduced facial expressions, depression, loss of taste and smell and ‘freezing’ (where someone suffers a temporary lack of ability to take a step, speak or communicate).
This highly individualised experience leads to difficulty in diagnosis, acceptance and on-going management. There is currently no cure for Parkinson’s so symptoms are managed through a combination of drugs and self-management (exercise, sleep hygiene etc.). The first year following diagnosis is involves many different healthcare professionals such as; Speech and Language Therapists, Dietitian’s, Occupational Therapists, Physiotherapists, a Parkinson’s Nurse Specialist and Neurology Specialist Consultants.
The provision of Parkinson’s services is complex and varied depending on provider. Services in the South West Peninsula cover acute and community settings, cross multiple regional and budgetary boundaries, cover a large geographical and rural area and have staffing pressures from unfulfilled roles, long term sick leave and increased patient numbers.

This project has had a different approach and an interactive style. It’s made me work with people who I would not normally interact with, we have worked with patients and their families. They have been at the heart of everything we have discussed and addressed. It’s been genuine co-design with patients.
Staff member, Sw peninsula parkinson’s service
Participants
- People living with Parkinson’s and their families and carers
- Parkinson’s Specialist Nurses
- Community care teams
- Therapy Specialists
- Consultant Neurologists
- Finance officer
- Parkinson’s UK Charity representative
To improve the patient and staff experiences of using and delivering services in the South West Peninsula, this project utilised a participatory design methodology to identify patient and provider needs and generate a series of solutions to these needs. A wide range of design research techniques were implemented that included; Lego® Serious Play®, Persona creation, Service Mapping and Prototyping.
Five full day workshops explored
- What are staff and user experiences?
- How is the service currently run?
- What could be different?
- Idea development
- Prototyping and Testing

Outcomes
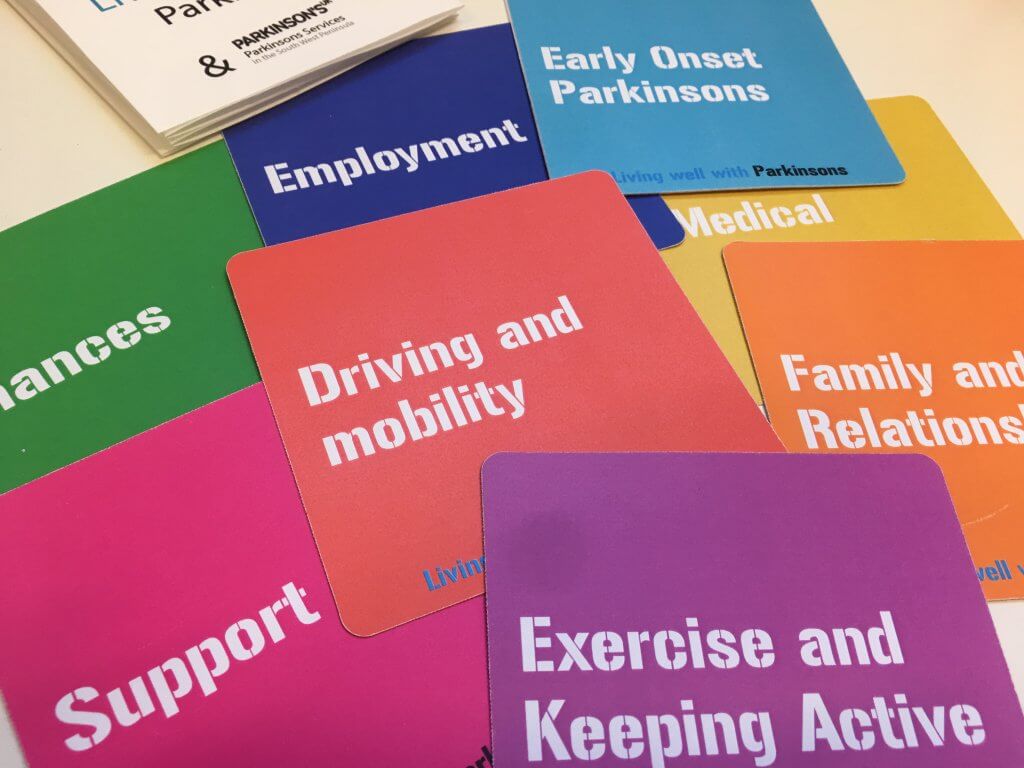
As a result of these workshops, five concepts are currently in development: A Parkinson’s Patient passport; New service and local information; a media campaign; a card deck to support therapeutic sessions; a self-management support and general information package. In addition further funding has been secured through The health Foundation to progress the development of a Home based Parkinson’s care service.

I’ve really enjoyed the exposure to different methods and ideas to support creative thinking. It’s challenged me to think outside the box
Person living with Parkinson’s
Next steps
This work informed a further project working with the Parkinson’s team, for more details, visit the project page for Plymouth Home Based Care Pathway
 to top
to top
